WHAT IS PERIODONTAL DISEASE?
Periodontal disease is the medical term for gum disease. It can be used to refer to the whole spectrum of gum disease, including gingivitis, which is a mild form of the condition, but is most often used to refer to the more severe, second stage of gum disease, periodontitis.
Periodontal disease is amongst the top ten most common diseases to affect humans1 and the leading cause of tooth loss for adults,2 so it’s important to be aware of the condition and how it can develop.
If you don’t put a stop to the first stage of periodontal disease, gingivitis, it can progress into periodontitis, a chronic inflammatory disease that affects the periodontium – the name given to the tissues, ligaments and bones that surround and support your teeth. If left untreated periodontitis can severely damage these structures3 eventually leading to tooth loss.
WHAT CAUSES PERIODONTAL DISEASE?
The type of bacteria that causes periodontal disease is aptly called periodontal bacteria. Normally, this bacteria doesn’t cause any problems, but under certain circumstances it can become harmful. This happens when the layer of bacteria and food particles, known as plaque, is not removed by regular brushing.4
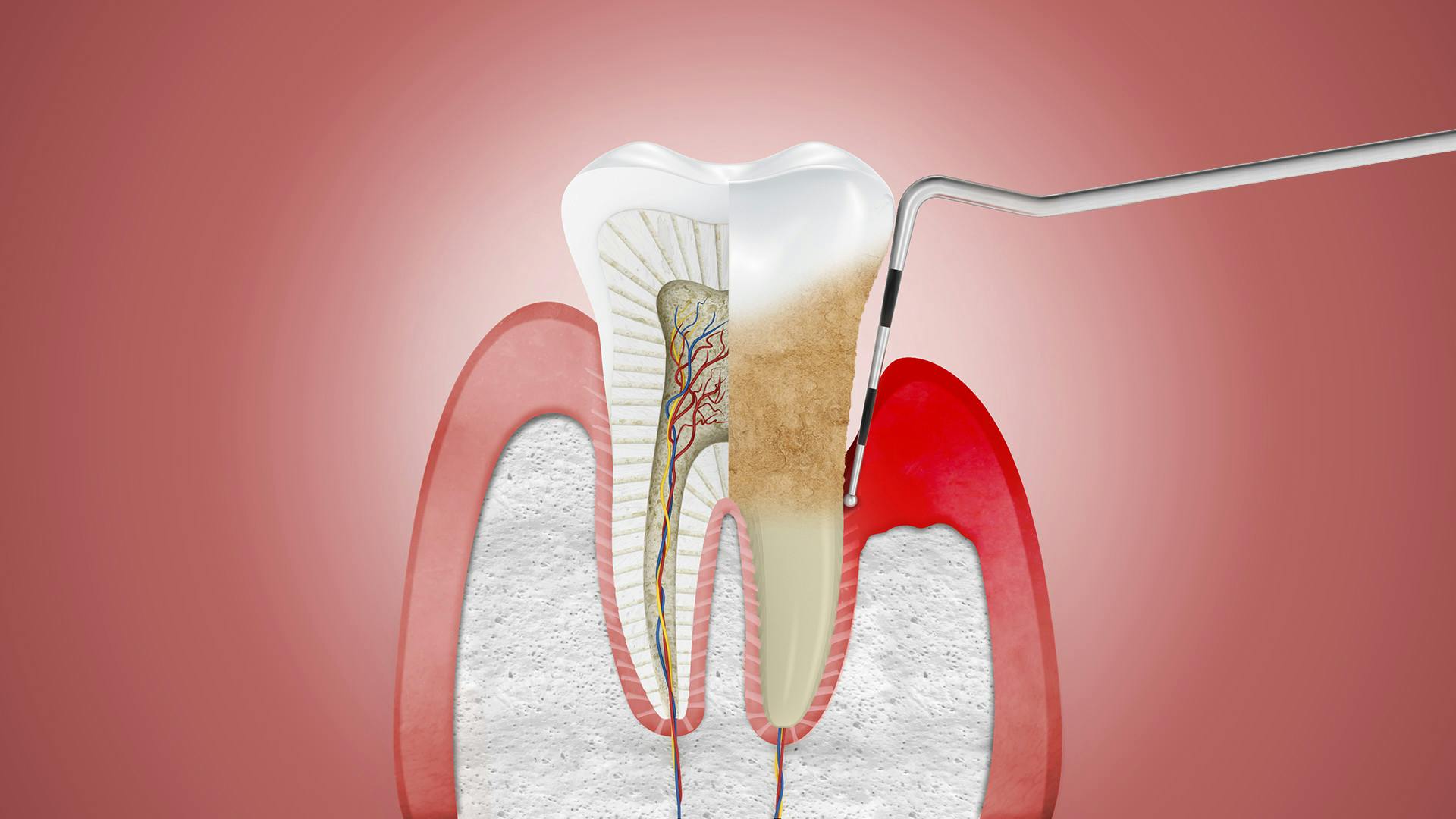
When plaque is left undisturbed, it creates a breeding ground for periodontal bacteria to multiply. This produces harmful by-products that set off your body’s natural inflammatory response, leading to swollen, inflamed gums. If this is left untreated periodontal disease can get worse as plaque hardens into tartar, a rough deposit that can’t be removed by brushing alone.5
As tartar develops it encourages more plaque growth towards the root of the teeth and inflammation can become chronic. Pockets form where the gum begins to detach from the tooth and, as harmful bacteria continues to grow in these spaces, infection spreads causing damage to the jaw bone and structures around the teeth, ultimately leading to tooth loss.6
PERIODONTITIS EXPLAINED7
It is vital to get treatment to stop periodontitis from getting worse. The first step is to visit your dentist, who can identify periodontal disease and advise you on the best way to treat it.
If you are diagnosed with periodontal disease you might see a specialist dentist called a periodontist. Periodontics focuses exclusively on gum disease and a periodontist is trained to prevent, diagnose and treat periodontal disease.
There are quite a few different periodontitis treatments available and your dentist, or periodontist, can explain which one is right for you. These could include:
- Advice on improving your oral health routine – if you are showing symptoms of gingivitis your dentist can help you to prevent it from progressing into more severe periodontal disease by explaining how to brush your teeth properly to remove plaque more effectively, or how to use dental floss and interdental brushes to clean hard to reach places. Your dentist may suggest using a daily toothpaste like parodontax, which, when used to brush twice daily, is effective at removing the build-up of plaque bacteria along the gum line (the area where the gum meets the tooth), helping to keep gums healthy and teeth strong.
- Professional cleaning – also called a scale and polish, where the dentist or hygienist scrapes away built up plaque and tartar and then polishes your teeth to discourage re-growth.
- Antibiotics – very occasionally these may be prescribed to clear up isolated infections that haven’t responded to other, non-surgical treatments.8
- Gum surgery – there are a few types of gum surgery that are used to treat periodontal disease. Your dentist may lift or cut back the gum to clean away deposits of plaque and tartar on the root surface, then polish this area to discourage regrowth. Or, if there is bone loss, your dentist may use a regenerative material (or graft) to treat this. After gum surgery, your dentist may recommend using a short course of antimicrobial mouthwash to help reduce bacteria and prevent infection.
In all cases your dentist should continue to monitor the progress of your periodontal disease, to ensure that you are getting the right treatment to help keep your gums as healthy as possible.
1 British Society of Periodontology. 2016. The Good Practitioner’s Guide to Periodontology. [ONLINE] Available at: https://www.bsperio.org.uk/publications/good_practitioners_guide_2016.pdf?v=3. [Accessed 31 July 2017]., 2 Periodontal (Gum) Disease . 2017. Periodontal (Gum) Disease . [ONLINE] Available at: https://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/GumDisease/. [Accessed 31 July 2017]., 3 British Society of Periodontology. 2016. The Good Practitioner’s Guide to Periodontology. [ONLINE] Available at: https://www.bsperio.org.uk/publications/good_practitioners_guide_2016.pdf?v=3. [Accessed 31 July 2017]., 4 What is Periodontitis - EFP. 2017. What is Periodontitis - EFP. [ONLINE] Available at: https://www.efp.org/patients/what-is-periodontitis.html. [Accessed 31 July 2017]., 5 What is Periodontitis - EFP. 2017. What is Periodontitis - EFP. [ONLINE] Available at: https://www.efp.org/patients/what-is-periodontitis.html. [Accessed 31 July 2017]., 6 What is Periodontitis - EFP. 2017. What is Periodontitis - EFP. [ONLINE] Available at: https://www.efp.org/patients/what-is-periodontitis.html. [Accessed 31 July 2017]., 7 What is Periodontitis - EFP. 2017. What is Periodontitis - EFP. [ONLINE] Available at: https://www.efp.org/patients/what-is-periodontitis.html. [Accessed 31 July 2017]., 8 British Society of Periodontology. 2016. The Good Practitioner’s Guide to Periodontology. [ONLINE] Available at: https://www.bsperio.org.uk/publications/good_practitioners_guide_2016.pdf?v=3. [Accessed 31 July 2017].